New ideas for improving diagnostics
Detecting viruses, bacteria, tumor markers or dangerous environmental toxins quickly and accurately saves lives. Two innovative projects funded by the Foundation in the corona context show what effective diagnostics could look like in the future.
Whether with glowing nanotubes or molecular tools - new diagnostic methods could deliver quick results and be available anywhere in the world.

Luminous Nanotubes instead of lengthy tests
Using a cotton swab, the paramedic carefully takes a sample from the elderly gentleman's nose. We have seen scenes like this many times on the news or have already experienced it firsthand: A swab from the nasopharynx is a prerequisite to detect the Sars-CoV-2 corona virus in a person's body. The genetic material of the virus is then detected in the sample by means of the so-called PCR method (very accurate, but time-consuming). Another method is to detect individual protein building blocks of the virus using a rapid antigen test (not quite as accurate, but fast).
Prof. Dr. Sebastian Kruss, Ruhr-Universität Bochum, has other plans. He wants to detect the presence of viruses like Sars-CoV-2 or bacteria by carrying out an investigation actually the body of the infected person or directly in blood or saliva samples – quickly and easily; no need for time-consuming sample preparation.
His research is still at the basic stage. But if Kruss and the other physicists, chemists and life scientists involved can keep up the good progress they have made so far, there will soon be unimagined new possibilities in diagnostics – thanks to tiny, luminous nanotubes. How does the method work, and where could it be used?
Sensors strike when viruses fall into "the trap"
At the heart of the new detection method are tiny carbon tubes of less than one nanometer in diameter. When these nanotubes, which can be obtained by burning methane, for example, are irradiated with light, they begin to glow. The human eye cannot see this glow because it is in the "near-infrared" and not in the visible light wavelength. However, special cameras can "read" the light signal that emanates from the thin tubes.
The nanotubes are the luminous components of a sensor. "Crucial to its function, however, is the organic phase around the tube, which can consist of antibodies or other detection molecules, for example," says Sebastian Kruss. The tubes are thus surrounded by a kind of "molecular adhesive layer" that can selectively recognize and bind viruses, bacteria or even their metabolic products.
As soon as a virus or bacterium enters the trap, i.e., is bound to the nanotube via the trapping molecule, the glow emanating from the tubes changes. This change appears as a positive test signal. However, if this glow remains unchanged, the suspected pathogens or substances are not present.
Where could the sensors be used?
The sensors, which can be imagined as a tiny tube or a noodle, can be used for laboratory tests, but also for detection in living organisms. Depending on which detection function the tiny tubes are equipped with, they can be used to detect various bacteria or viruses, but also signal substances, tumor markers, antibodies, blood sugar, neurotransmitters, insulin or other hormones.

In Sebastian Kruss' laboratory, nanosensors are excited with green light under a fluorescence microscope.
One advantage of the method is its speed.
One advantage of the method is its speed. The result is available almost immediately. Blood, urine or saliva samples could be dripped onto the sensors to detect pathogens or biomarkers that indicate an infection, inflammation or even a tumor condition. "Nanosensors could also, for example, speed up the diagnosis of sepsis, a life-threatening condition in which every minute counts," explains biophysicist Kruss. Of particular interest is that the sensors could be applied directly to artificial hip joints or even catheters, for example. Once these "spare parts" or medical devices are in the human body, it is difficult to notice whether dangerous bacteria have settled as biofilm on the materials used.
A nanosensor on the artificial joint, however, would immediately "strike" as soon as unwanted bacteria begin to spread. "The advantage of the technology is that the nanotubes glow in the near-infrared range, a range that remains virtually undisturbed by background signals emanating from the surrounding tissue," says Sebastian Kruss. The optical signal can penetrate body tissue up to one centimeter because it is hardly absorbed or scattered by water, cells or blood. A camera could then "look" through the intact skin into the body and capture the signal sent by the sensors.
Kruss is currently working on a prototype of such a camera with a team at the Fraunhofer Institute for Microelectronic Systems and Circuits in Duisburg. In principle, however, the light signal could also be captured by a cell phone camera. This application on a cell phone might sound a bit like science fiction, but it is not so improbable that one day we could find out whether or not we are infected with Sars-CoV-2 or other pathogens with the help of a corresponding nanotube test kit and an app on our smartphone.

Diagnostics for all – LAMP-PCR
Anyone in this country who orders the molecular ingredients for the laboratory detection of viruses or bacteria usually receives the enzymes and reagents they need the very next day. "If, on the other hand, colleagues at our partner university in Addis Ababa request these test enzymes from the manufacturers, they usually have to wait one to two months for them and pay three to four times the price," says Johannes Kabisch, a professor at Darmstadt Technical University. In a cooperative project with researchers at the University of Cambridge and the Ethiopian Biotechnology Institute, Kabisch is working to address this disgraceful state of affairs: How can the molecular tools needed for viral diagnostics, for example, be produced in countries with scarce resources? "We want to take the technology to where it is needed," says the biotechnologist, outlining one of the project's core ideas.
His approach: On the one hand, instead of the classic PCR test for detecting viruses or other pathogens, a somewhat modified method known as "LAMP PCR" is used that is faster, simpler and cheaper. Secondly, the enzymes needed for the test, or the genetic blueprint, are not subject to a patent, but come from the Cambridge-based "Open Enzyme Collection," a "Wikipedia for enzymes," Johannes Kabisch explains. "The University of Cambridge's Open Bioeconomy Lab supports the project not only through its database of patent-free gene sequences for biomolecules, but also through its experience and networks with biotechnology laboratories in the global south."
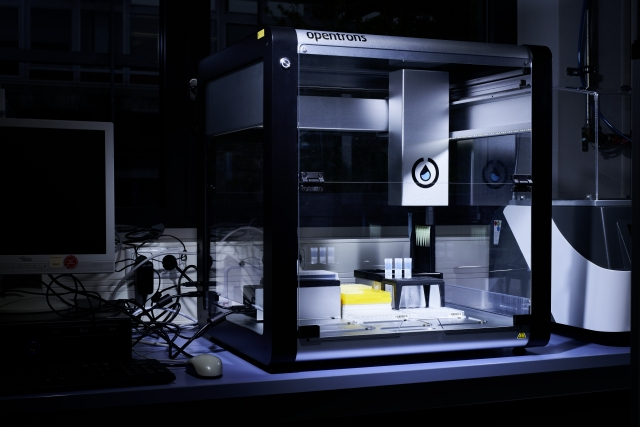
Johannes Kabisch uses a pipetting robot for virus tests in the laboratory. The aim of the project, however, is to track down pathogens with as little high-tech as possible. From summer 2021, the biologist will continue his research at the NTNU in Trondheim.
n theory, you [...] just need a water bath.
A quick yes or no: the LAMP-PCR
The PCR (polymerase chain reaction) multiplies the genetic information of the suspected pathogens, or sections of it, and finally makes it visible in the examined sample by multiple copying and staining. In the commonly used, classical PCR, high and low temperatures alternate; because of this, a so-called thermocycler is required. "LAMP PCR, on the other hand, runs at a constant temperature. In theory, you don't need an expensive device to perform it, just a water bath that keeps the temperature at 63 degrees Celsius," Kabisch explains. With this test, a positive result can be detected by a color change in the sample after just half an hour. With classical PCR, it takes about three to 24 hours for the result to be established.
Until now, however, LAMP PCR was clearly inferior to the classical variant. It was not as robust and not as sensitive. The method has since been improved by researchers worldwide. "LAMP PCR gives a reliable yes or no answer, indicating whether the sample contains the suspected pathogen or not," Kabisch says. In future, the technique could become a good alternative to the classical PCR method. However, it does not provide exact information about the amount of viruses or bacteria contained.
Bioproduced enzymes are key
The enzymes needed for LAMP PCR are produced by bacteria of the Bacillus subtilis variety. The genetic material of these bacteria is genetically modified to produce the enzymes "reverse transcriptase" or a "polymerase".
...the bacteria do all the work
The first enzyme is needed for the detection of RNA viruses such as Sars-CoV-2. It translates RNA into DNA, which can then be amplified with the second enzyme, a kind of molecular copier, and thus made visible. Bacteria also produce these enzymes in a conventional production process. However, they are then purified from the disrupted bacterial cells. "In the production method we have chosen, the bacteria do all the work," says Johannes Kabisch. They make the enzymes and are then induced to enter a steady state, the bacterial spore, by altering culture conditions. The key feature of this technique is that "the spore carries the desired enzyme on its surface, it even kills its mother cell itself, and a simple centrifugation is all that is needed to purify the enzymes attached to the spores," says the researcher from Darmstadt.
The enzymes are not only easier to purify and cheaper to produce, they are also more stable because they are attached to the spores and last for about three months even at room temperature. However, before enzymes derived from such bioproduction arrive in diagnostics, all sorts of fine-tuning work must be done, test protocols must be checked and found to be reliable. Kabisch is confident: "By carefully adjusting the production process and testing the obtained enzymes, we will be able to develop reliable test systems". Following a successful transfer of knowledge from Darmstadt and Cambridge, he hopes to be able to produce enough enzymes in Addis Ababa for 10,000 prototypes of a Sars-CoV-2 test kit in the not-too-distant future.